Herzliya Medical Center
Tel: +972-9-959-4888
09:00-18:00
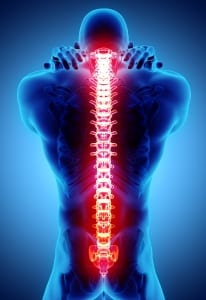 The cervical spine has a total of seven vertebrae. This is a relatively fixed group of vertebrae, which does not move significantly. Its upper vertebrae are connected to the skull, and due to their unique structure, contribute to the neck’s ability to move freely. Severe problems affecting the cervical spine are typically rare (especially in comparison with the lower back), but do sometimes occur. There are even instances in which cervical fusion surgery is needed – a delicate surgical procedure performed at Herzliya Medical Center Hospital by internationally renowned spinal orthopedic specialists.
The cervical spine has a total of seven vertebrae. This is a relatively fixed group of vertebrae, which does not move significantly. Its upper vertebrae are connected to the skull, and due to their unique structure, contribute to the neck’s ability to move freely. Severe problems affecting the cervical spine are typically rare (especially in comparison with the lower back), but do sometimes occur. There are even instances in which cervical fusion surgery is needed – a delicate surgical procedure performed at Herzliya Medical Center Hospital by internationally renowned spinal orthopedic specialists.
As stated above, severe problems that are not solved by conservative treatment – massage, chiropractic and the like – are considered to be relatively rare so far as the cervical spine is concerned. Therefore, operations of this area are also considered to be relatively rare, but they do exist.
Cervical fusion surgery is performed when the medical team comes to the conclusion that there is a substantial problem in this area, which cannot be solved in any other way. Such problems are divided into two types: significant weakness of the cervical vertebrae, or danger anticipated for one of the nerves in the area, due to the existing structure of the vertebrae and the discs between them.
As a rule, there are three specific medical conditions that typically lead to performing such an operation:
Before describing in depth how the fusion itself is performed, we first note that there are two main methods for performing the operation:
Apart from these two methods, the surgeon also has an additional method at his disposal – minimally invasive fusion surgery. This method enables the operation to be performed via a few tiny openings in the skin (only half a centimeter in size). It usually ensures more rapid recovery, but is not suitable for every patient.
After the physician decides on the method by which the operation will be performed (the decision, incidentally, is made also based on the diagnosis, the nature of the problem and your physical condition), and after a date is set for the operation itself, all that remains is to perform the actual procedure.
The operation is, of course, performed under general anesthesia. In its course, up to four vertebrae can be fused together, depending on the extent of the problem, which, of course, influences the duration of the operation. The actual fusion is achieved with the help of a bone graft (usually taken from the parts of the vertebrae removed in the operation itself, but sometimes from an external donor), with the addition of special metal fixation. The metal fixation enables the bones to “fuse” into each other naturally, thus becoming stronger, without risking structural breakdown.
In the initial days after the operation, you will, of course, be somewhat limited – depending on the method by which the surgical procedure was performed. You may be asked to wear a “Philadelphia collar” for several days, in order to ensure that the treated area does not move and will not undergo sharp movements. After a few days, you will be required to wear this collar only when travelling, for a few months.
As a rule, the operation should not have a large effect on your movement ability, since the upper vertebrae of the spine do not usually move very much (their role is mainly to provide the head and neck with stability). If more than two vertebrae were fused together, you may feel some limitation, and this may disappear with time.
In the initial months after the operation, you will be called in for follow-up with your surgeon, in order to ensure that the operation was performed in the best way possible and achieved the required results. The specialist physicians at Herzliya Medical Center Hospital are careful to follow the patient even a long time after being discharged from the medical center, in order to ensure that he recovers optimally.
For advice and further information, contact us at telephone: +972-9-959-4888, or leave your details and we will get back to you promptly.
Contact details