Herzliya Medical Center
Tel: +972-9-959-4888
09:00-18:00
The aorta is the largest blood vessel in the body. Its diameter in an adult is about 2.5 cm – similar to a garden hose. This blood vessel provides blood to all body organs from the heart. In certain conditions, the aorta could grow beyond its normal diameter. This condition is called an aneurysm. This expansion of the aorta could cause its wall to tear, leading to deadly bleeding that ends in most cases in death. However, when an aneurysm is diagnosed on time, these severe events can be prevented via repair surgery; aorta surgery. Like in many conditions in medicine, early diagnosis is the foundation for successful treatment.
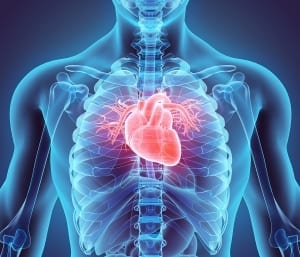
The aorta is shaped like a cane. Its root is in the heart and after a short course in the thorax (the ascending aorta), it curves back (aortic curve). From here, the aorta descends along the spine in the thorax and abdomen (thoracic abdominal aorta). Most aortic aneurysms (about 75%) are in the abdominal part. A quarter of them is located in the thorax, and these aneurysms are more dangerous, and their tearing usually leads to grim results.
Aortic aneurysms are usually caused by damage in the aortic wall. Their source is usually Atherosclerosis caused by choleste
rol accumulation and other fatty deposits on the vascular walls. This condition is exacerbated in the presence of other diseases like hypertension, diabetes, and smoking. However, there are also congenital conditions where there is a weakness of vascular walls in the body. In these conditions, aortic aneurysms might develop in younger people – in the first decades of their life.
Most aortic aneurysms are discovered at random. They don’t cause any effects. In fact, their vast majority is discovered during a chest x-ray or CT that is done to investigated another medical issue. However, effects arising from localized pressure by the expanded aorta of adjacent organs are possible. A tear of the aortic wall is a deadly condition usually expressed by a sharp pain in the chest, back or abdomen.
A thoracic aortic aneurysm can be diagnosed via non-invasive tests like an echocardiogram (ultrasound of the heart and large blood vessels, CT or MRI (magnetic resonance imaging). These tests have the highest accuracy rating, and they provide information about the aorta’s diameter and the existence of other diseases.
Treatment of aortic aneurysms depends on the size and location of the aneurysm. In general, if the aneurysm is small and the patient doesn’t have related effects, monitoring alone is standard with imaging tests in fixed intervals. The purpose of these tests is to evaluate any change of the aneurysm’s size. If the aneurysm’s diameter exceeds 5 cm, or alternatively its growth rate exceeds 1 cm per year, there is an indication for surgery. Of course, the risk versus benefit must be evaluated in every patient when performing the surgical action.
The standard treatment of thoracic aortic aneurysms is a surgical repair of the aneurysm and replacing the sick aortic segment with a Dacron synthetic implant. This implant has an unlimited lifespan, it isn’t rejected by the body and doesn’t require taking anticoagulants.
During the aorta surgery, the patient is connected to a heart-lung machine, similar to many heart surgeries. This machine, as per its name, performs the functions of the heart and lungs so that their activity can be stopped. However, in contrast to regular heart surgery, in thoracic aortic replacement surgery, there is a need to stop the blood flow in the body completely. For that purpose, the patient’s body is cooled to a low temperature of about 15-20 Celsius. In this temperature, the different body organs’ oxygen needs are reduced and stopping the blood flow to these organs is more tolerated. The timeframe in which the blood supply is stopped is limited, and it’s recommended not to exceed 50 minutes, so the operation is performed with time limitations and racing against the clock. Since the brain tissue is more sensitive to a lack of oxygen, during the surgery, and when the heart-lung machine is stopped, the surgeon makes sure to selectively provide blood to the brain. In order to make sure not cerebral damage is caused, the surgical staff uses advanced monitoring devices providing information about the oxygen level in the brain, the speed of the blood flow to the brain and the brain’s electric activity.
In recent years, there is another treatment approach to aortic aneurysms. This approach is based on stent implantation in the infected aorta area. The advantage of this method is in it being minimally invasive. It doesn’t involve a large surgical incision, connection to a heart-lung machine and the discontinuation of blood flow in the patient’s body. However, this method is limited to only certain areas in the aorta, and the long term results are unknown.
An increase in awareness of aortic diseases among the public and medical staff can lead to early detection and planned surgical treatment, and thus saving a life.